BAYESIAN DOSING
How does it work?
Bayesian dosing uses patient data and laboratory results to estimate a patient’s ability to absorb, process, and clear a drug from their system. Using a published population model, Bayesian dosing tools adjust the pharmacokinetic / pharmacodynamic parameters so that a patient-specific, individualized drug model (that describes the patient-specific results accurately) is created. This individual model is then used to provide a patient-specific dosing recommendation to reach a therapeutic target.
Bayesian dosing, however, also takes into account the likelihood that a given laboratory result is real, versus being incorrectly recorded, an assay error (or any other residual error). In practice, this means that Bayesian dosing tools require more ‘convincing’ that an extreme patient really does excrete the drug that quickly, for example. Until there is sufficient supportive evidence, these tools will tend towards the mean when calculating this individual patient’s excretion rate. We call Bayesian dosing as such because of this concept of an underlying population prior distribution of these parameters, such as excretion for example.
For patients where you have no laboratory results yet available, some tools support the use of a population model with individual patient details (age, height, weight, sex, even genotype if available) to calculate an initial dose estimate. Although this is not as accurate as a Bayesian dose recommendation, this is known to be superior to clinical experience-based dosing (Matthews et al., 2004).
Where has it been used?
Bayesian dose forecasting has been used extensively around the world, but its use in a clinical setting (where magnitude of benefit has been systematically studied – see here) has been previously isolated to pockets of clinicians who were familiar with the technology and had a good understanding of both IT and mathematics. It is used in hospitals such as St Jude’s, The Mater (Brisbane), St Vincent’s (Sydney), Christchurch Hospital, a variety of Melbourne teaching hospitals, Cincinnati, USC and The Hague Hospital network.
Pharmacogenomics – one more step toward precision medicine
Pharmacogenomics is the study of how genes affect individual response to drugs and is an important part of precision medicine. Variability between patients though, is also caused by differences in diet, exercise, epigenetics, interacting medications, and more. Ultimately, we can achieve optimum outcomes by combining pharmacogenomic data with pharmacokinetic and pharmacodynamic data that reflects these other factors to most accurately dose patients.
For example, warfarin is known to be strongly affected by genotype and haplotype (as well as diets, other medications, and more). The safe dose is known to vary seven-fold depending on genotype (CYP2C9) and haplotype (VKORC1). The author of this post happens to have an unusual VKORC1 haplotype – essentially needing half the dose of the average person in the population. With overdose of warfarin directly linked to haemorrhagic events, personally, this matters.
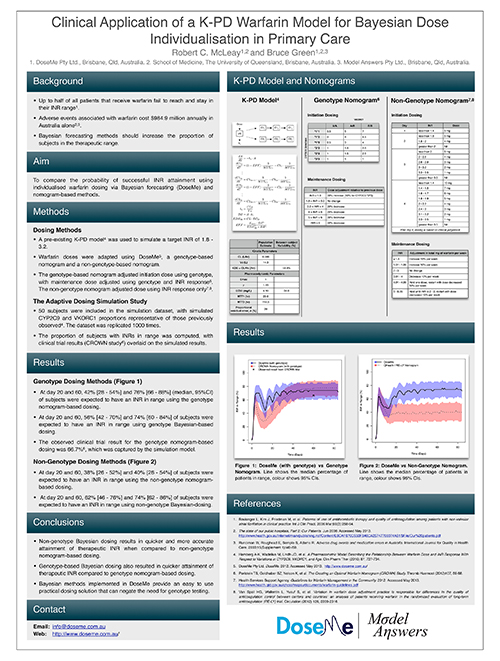
The poster to the right shows work performed by DoseMeRx, investigating genotype-led individualised warfarin dosing. DoseMeRx was able to bring patients into the therapeutic range more rapidly when genotype was known – and as this directly impacts hospital stay length, the cost benefits are obvious.
Genomic information is, and will remain, very useful for drug selection, cancer therapy, and more. We’re at the beginning of routine use of genomics in dosing other medications, with some of DoseMeRx’s hospitals beginning to genotype patients. The exciting future of pharmacogenomics is just beginning.
— Robert McLeay, PhD
CSO, DoseMeRx.
Further/Extension Reading:
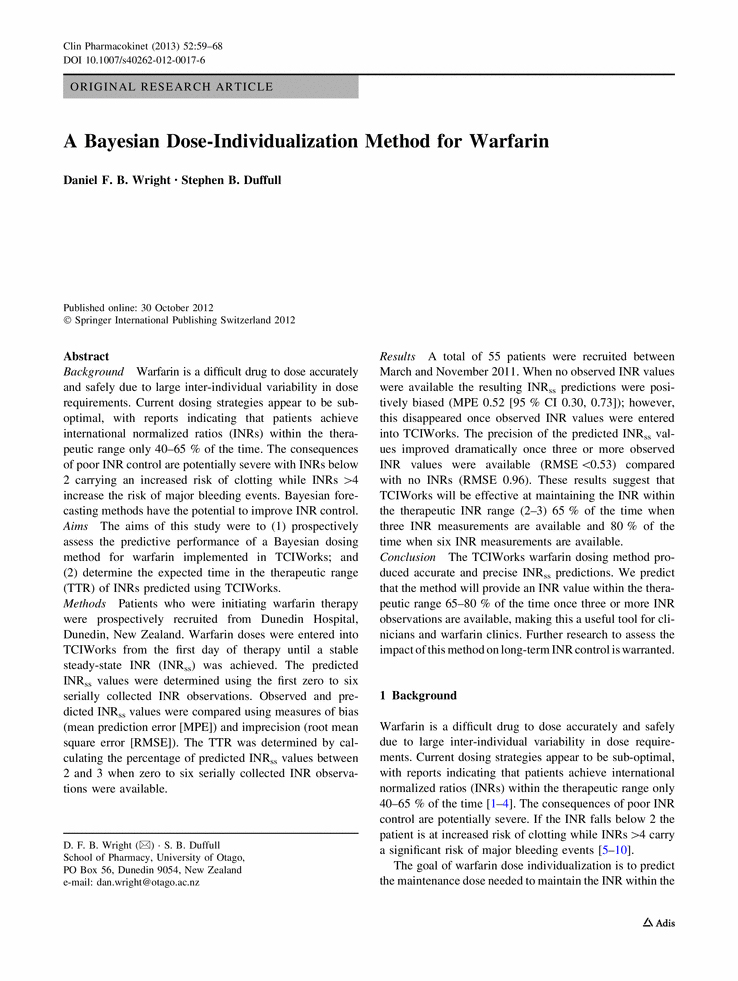
For a deeper look at Bayesian dose individualization, we would recommend the following papers:
- Burton, ME. et al. A Bayesian feedback method of aminoglycoside dosing. Clinical pharmacology and therapeutics, 1985:37, 349-357.
- Thomson, A. H. & Whiting, B. Bayesian parameter estimation and population pharmacokinetics. (Review). Clinical pharmacokinetics 1992:22, 447-467
- Sheiner, L. B. Computer-aided long-term anti-coagulation therapy. Computers and Biomedical Research, 1969:2, 507-518
Burton et al. would be a recommended introduction to the mathematics of Bayesian dose individualization, with Thomson et al. being a useful review of the area. As you can see from the last paper, Bayesian dosing has been around for quite some time.
Warfarin – Genotype vs Bayesian
DoseMe attended PAGE2013, where we had a software demonstration booth and a scientific poster. The below poster shows the difference between using genotype or not when dosing warfarin: